Flecainide Induced Refractory Ventricular Arrhythmia in A Hypertrophic Cardiomyopathy Patient
Athanasios Saplaouras*, Panagiotis Mililis, Antigoni Sakellaropoulou, George Bazoukis, Athena Batsouli, Fotios Toulgaridis, Michael Efremidis, Konstantinos Letsas
Second Department of Cardiology, “Evangelismos” General Hospital of Athens, Greece
*Corresponding author: Athanasios Saplaouras, MD, MSc, Department of Cardiology, General Hospital of Athens “Evangelismos”, Ipsilantou 47, Athens, Postal code: 10676, Greece. Tel: +306974302988; Email: saplaouras@hotmail.com
Citation: Saplaouras A, Mililis P, Sakellaropoulou A, Bazoukis G, Batsouli A (2020) Flecainide Induced Refractory Ventricular Arrhythmia in A Hypertrophic Cardiomyopathy Patient. Annal Cas Rep Rev: ACRR-107.
Received Date: 31 March, 2020; Accepted Date: 06 April, 2020; Published Date: 10 April, 2020
Abstract
Herein we present a 55-years-old male with end-stage hypertrophic cardiomyopathy and implantable cardioverter defibrillator that developed life threatening ventricular arrhythmia after the administration of flecainide. The patient experienced many appropriate shocks until the arrhythmia was successfully terminated.
Keywords: Proarrhythmia, flecainide, ICD, HCM.
Introduction
Flecainide is a class 1C antiarrhythmic agent blocking sodium channels with use dependent prolongation of phase 0 in the fast response cardiac myocyte, a favorable property in the management of supraventricular tachycardias (SVT) including atrial fibrillation (AF) [1]. Flecainide is recommended as one of the first line therapies for pharmacological conversion as well as maintenance of sinus rhythm in patients with atrial fibrillation [2]. Nevertheless, based on the Cardiac Arrhythmia Suppression Trial (CAST) study results, flecainide is not recommended in patients with structural heart disease due to high proarrhythmic risk [3].
Case
A 55-years-old male with past medical history of hypertrophic cardiomyopathy (HCM), Implantable Cardioverter Defibrillator (ICD) and paroxysmal atrial fibrillation (PAF), was transferred in the emergency department due to a transient loss of consciousness after having experienced multiple shocks. The patient stated that the symptoms of AF started 48 hours prior to presentation, and that flecainide acetate was prescribed to him by an out-of-hospital medical doctor. The initial ICD interrogation (Fortify Assura DR; St Jude Medical) revealed an episode of ventricular tachycardia that was cardioverted with a direct current (DC) shock and an episode of ventricular tachycardia (VT) that rapidly deteriorated to Ventricular Fibrillation (VF) refractory to DC shocks at 20J and 30J and was successfully terminated after the third DC shock was delivered at 38J (Figure 1). The patient’s baseline electrocardiogram revealed sinus rhythm with ventricular pacing (Figure 2). The echocardiogram showed characteristics of “burned-out” HCM with ejection fraction 40% and dilated left ventricle [4]. The patient was treated with sodium bicarbonate 8% according to previous experience and remained stable without any new episode [5]. His vital signs were stable and his laboratory tests were unremarkable with no evident electrolyte disturbances. The next day, our patient underwent coronary angiography that revealed coronary arteries without any angiographically significant stenosis. Finally, he was discharged on day 4 without any arrhythmiological event during his hospitalisation, after appropriate programming of the ICD.
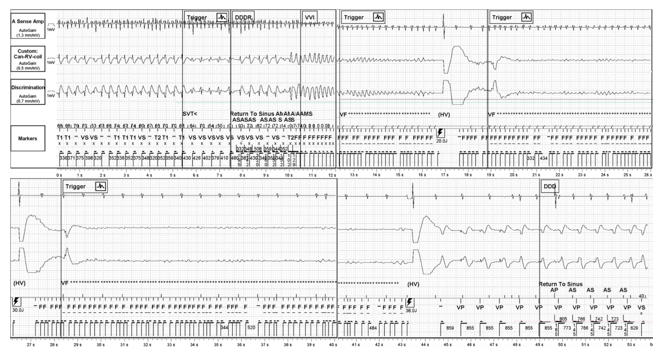
Figure 1: Atrial electrogram (EGM) showing AF and ventricular EGM showing VT that deteriorated to VF. Atrium was cardioverted to sinus rhythm after the second shock. Refractory VF was successfully terminated after the third shock was delivered (38J).
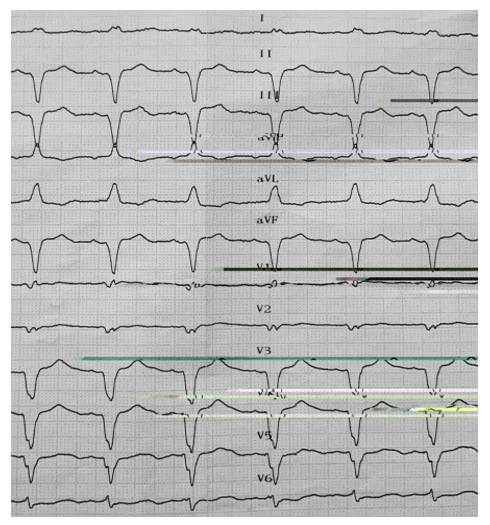
Figure 2: Baseline electrocardiogram showing sinus rhythm with ventricular pacing.
Discussion
The main consideration prior to flecainide administration is to rule out the presence of structural heart disease and ischemic cardiomyopathy in order to avoid the associated increased risk of proarrhythmia. The early sign of flecainide ventricular proarrhythmia, which usually manifests as polymorphic ventricular tachycardia or fibrillation, is QRS prologation. The warning of flecainide’s proarrhythmia was mainly formulated on the basis of the CAST according to which flecainide is associated with increased mortality when administered to patients with prior myocardial infarction [3], [6], [7]. Herein we present a patient that has medical history of HCM with moderate left ventricular dysfunction and left ventricular dilation to whom flecainide was administered due to PAF. There is lack of evidence about the potential benefit from flecainide treatment in patients with ICD, given that ICDs ameliorate the proarrhythmic risk. Nevertheless, our patient developed ventricular arrhythmia refractory to the first two delivered DC shocks, probably associated with flecainide administration. It has been previously reported that the amount of energy required to terminate a VF is higher in animals treated with cardiac sodium channel blockers, although it’s controversial according to findings of flecainide defibrillation threshold alteration in pigs [8], [9]. In our patient 20J and 30J DC shocks were ineffective in terminating ventricular fibrillation and 38J shock successfully treated the arrhythmia. The clinical presentation of an electrical storm can be dramatic and life-threatening. For this reason, class Ic antiarrhytmic drugs should not be considered as an alternative treatment to AF in the presence of structural heart disease even in patients with ICD.
References
- Holmes B, Heel RC (1985) Flecainide A Preliminary Review of its Pharmacodynamic Properties and Therapeutic Efficacy. Drugs 29: 1-33.
- Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, et al. (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. European Heart Journal 37: 2893-2962.
- Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, et al. (1991) Mortality and Morbidity in Patients Receiving Encainide, Flecainide, or Placebo. New England Journal of Medicine 324: 781-788.
- Biagini E, Coccolo F, Ferlito M, Perugini E, Rocchi G, et al. (2005) Dilated-hypokinetic evolution of hypertrophic cardiomyopathy: prevalence, incidence, risk factors, and prognostic implications in pediatric and adult patients. Journal of the American College of Cardiology 46: 1543-1550.
- Goldman MJ, Mowry JB, Kirk MA (1997) Sodium bicarbonate to correct widened QRS in a case of flecainide overdose. The Journal of Emergency Medicine 15: 183-186.
- Friedman PL, Stevenson WG (1988) Proarrhythmia. The American Journal of Cardiology 82: 50N-58N.
- Naccarelli GV, Wolbrette DL, Luck JC (2001) Proarrhythmia. Medical Clinics of North America 85: 503-526.
- Hernandez R, Mann DE, Breckinridge S, Williams GR, Reiter MJ (1989) Effects of flecainide on defibrillation thresholds in the anesthetized dog. Journal of the American College of Cardiology 14: 777-781.
- Natale A, Jones DL, Kleinstiver PW, Kim Y-H, Wood GK, et al. (1993) Effects of Flecainide on Defibrillation Threshold in Pigs. Journal of Cardiovascular Pharmacology 21: 573-577.
